Cataract
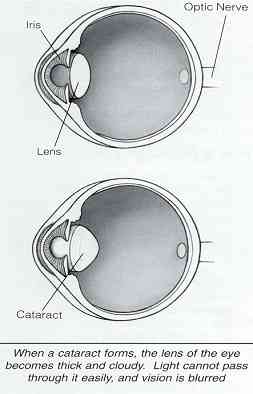
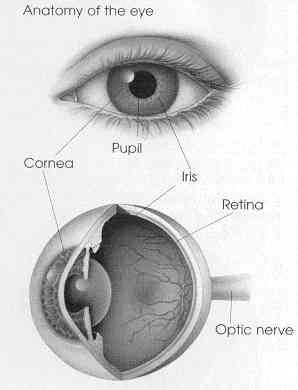
A cataract is a clouding of the normally clear lens of the eye. The lens focuses light rays on the retina at the back of the eye to produce a sharp image of what we see. When the lens becomes cloudy, the light rays cannot pass easily through it, and the image becomes blurry.
Cataracts usually develop as part of the aging process, but can also come from:
- Eye injuries
- Certain diseases
- Medications
- Genetic inheritance
The cataract may need no treatment at all if the vision is only a little blurry. A change in your eyeglass prescription may improve vision for a while.
There are no medications, eye drops, exercises or glasses that will cause cataracts to disappear once they have formed. When you are not able to see well enough to do the things you like to do, cataract surgery should be considered. Surgery is the only way to remove a cataract.
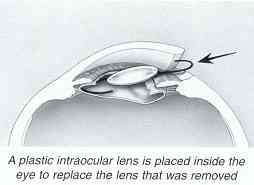
Cataracts cannot be removed with a laser, only through a surgical incision. In cataract surgery, the cloudy lens is removed from the eye. In most cases, the focusing power of the natural lens is restored by replacing it with a permanent intraocular lens implant.
How is the surgery done?Under an operating microscope, a small incision is made into the eye. Microsurgical instruments are used to fragment and suction the cloudy lens from the eye. The back membrane of the lens (called the posterior capsule) is left in place.
A plastic intraocular lens implant will be placed inside the eye to replace the natural lens that was removed. The incision is usually self-sealing without stitches.
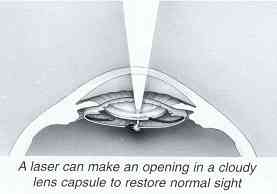
When is laser used?The posterior capsule sometimes turns cloudy several months or years after the original cataract operation. If this blurs your vision, a clear opening can be made painlessly in the center of the membrane with a laser. Laser surgery is never part of the original cataract operation.
Will cataract surgery improve my vision?Over 95% of cataract surgeries improve vision. Complications are rare, but your eye doctor will monitor for them following the procedure.
Even if the surgery itself is successful other problems with the eye, such as macular degeneration (aging of the retina), glaucoma and diabetic damage may limit vision after surgery. Even with such problems, cataract surgery may still be worth-while.
If the eye is healthy, the chances are excellent that you will have good vision following removal of your cataract.
What can I expect if I decide to have surgery?Before surgery
When you and your eyecare provider have decided that you will have your cataract removed, be sure to mention any special medical risks you may have. Ask your eyecare provider if you should continue your usual medications.
Your eye will be measured to determine the proper power of the intraocular lens that will be placed in your eye during surgery.
The day of surgery
Surgery is usually done on an outpatient basis. You may be asked to skip breakfast, depending on the time of your surgery. Upon arrival for surgery, you will be given eyedrops, and perhaps medications to help you relax.
A local anesthetic will make the operation painless. You will be awake during the procedure and you will be able to see light and movement. You do not have to worry about keeping your eye open or closed.
The skin around your eye will be thoroughly cleaned, and sterile coverings will be placed around your head. When the operation is over, the surgeon may place a shield over your eye.
After a short stay in the outpatient recovery area, you will be ready to go home. You should plan to have someone else drive you home.
Following surgery
- Use the eye drops as prescribed
- Be careful not to rub or press on your eye
- Use over-the-counter pain medicine if necessary
- Avoid very strenuous activities
- Continue normal daily activities
- Ask your doctor when you can begin driving
- Wear eyeglasses or shield as advised by your doctor
You will have several post operative visits following the procedure to monitor the recovery of the eye. In most cases the recovery is quick and painless. The procedure changes your eyeglass prescription and often reduces or eliminates the need for eyeglasses for distance vision. New eyeglasses are usually prescribed about a month after the procedure.
You may choose to have either the surgeon or your Optometrist perform your post-operative care. The three surgeons that perform cataract surgery at Uvalde Memorial Hospital all live in San Antonio. You will be given the option of continuing your care with your Optometrist once the surgeon feels that your eye is stable. One of the Optometrists at The Eye Center of Uvalde is on call 24 hours a day, seven days a week. If a complication should occur that needs additional treatment by your surgeon, you may have to travel to San Antonio for that procedure.
Surgical Options
Oday Alsheikh, M.D. is a board certified corneal specialist.
Dr. Alsheikh performs cataract surgery at the Ocular Surgery Center in San Antonio and at Uvalde Memorial Hospital. All pre-operative and post operative care can be provided at The Eye Center of Uvalde.
Detached & Torn Retinas
The retina is a nerve layer at the back of your eye that senses light and sends images to your brain. An eye is like a camera. The lens in the front of the eye focuses light onto the retina. You can thin of the retina as the film that lines the back of a camera.
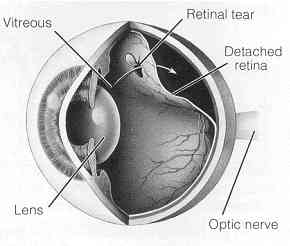
What is a retinal detachment?A retinal detachment occurs when the retina is pulled away from its normal position. The retina does not work when it is detached. Vision is blurred, like a camera picture would be blurry if the film were loose inside the camera.
A retinal detachment is a very serious problem that almost always results in blindness unless it is treated.
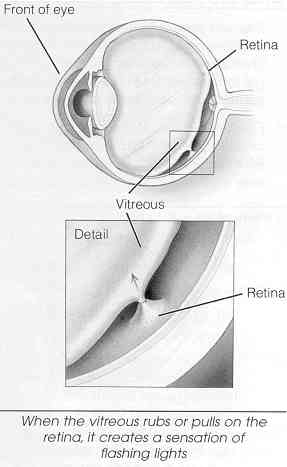
What causes retinal detachment?The vitreous is a clear gel that fills the middle of the eye. As we get older, the vitreous may pull away from is attachment to the retina at the back of the eye.
Usually, the vitreous separates from the retina without causing problems. But sometimes the vitreous pulls hard enough to tear the retina in one or more places. Fluid may pass through the retinal tear, lifting the retina off the back of the eye, like wallpaper can peel off a wall.
The following conditions increase the chance that you might get a retinal detachment:
- Nearsightedness
- Previous cataract surgery
- Glaucoma
- Severe injury
- Previous retinal detachment in your other eye
- Family history of retinal detachment
- Weak areas in your retina that can be seen by your eye care provider
These early symptoms may indicate the presence of a retinal detachment:
- Flashing lights
- New floaters
- A gray curtain moving across your field of vision
These symptoms do not always mean a retinal detachment is present; however, you should see your eye care provider as soon as possible.
Your eye care provider can diagnose retinal detachment during an eye examination. Some retinal detachments are found during routine eye examination.
Only after careful examination can your eye care provider tell whether a retinal tear or early retinal detachment is present.
What treatment is needed? Retinal TearsMost retinal tears need to be treated with laser surgery or cryotherapy (freezing), which seals the retina to the back wall of the eye. These treatments cause little or no discomfort and may be performed in your eye care provider’s office. Treatment usually prevents retinal detachment. In some cases retinal tears can be observed without treatment.
Retinal DetachmentsAlmost all patients with retinal detachments require surgery to put the retina back in its proper position.
Types of surgeryThere are several ways to fix a retinal detachment. The decision of which type of surgery and anesthesia (local or general) to use depends upon the characteristics of your detachment.
In each of the following methods, your eye care provider will locate the retinal tears and use laser surgery or cryotherapy around them to seal the tear.
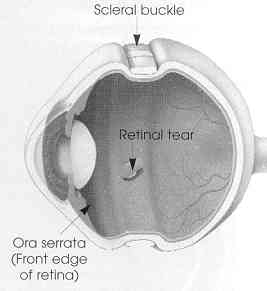
Scleral Buckle
A flexible band (scleral buckle) is placed around the eye to counteract the force pulling the retina out of place.
The eye care provider often drains the fluid under the detached retina from the eye, pulling the retina to its normal position against the back wall of the eye. This procedure is performed in an operating room.
Pneumatic retinopexy
A gas bubble is injected into the vitreous space inside the eye. The gas bubble pushes the retinal tear closed against the back wall of the eye.
Your eye care provider will ask you to maintain a certain head position for several days. The gas bubble will gradually disappear.
Vitrectomy
The vitreous gel, which is pulling on the retina, is removed from the eye and usually replaced with a gas bubble. Your body’s own fluids will gradually replace the gas bubble.
After surgeryYou can expect some discomfort after surgery. Your eye care provider will prescribe any necessary medications for you and advise you when to resume normal activity. You will need to wear an eye patch for a short time. Flashing lights and floaters may continue for a while after surgery.
If a gas bubble was placed in your eye, your eye care provider may recommend that you keep your head in special positions for a time. DO NOT FLY IN AN AIRPLANE OR TRAVEL UP TO HIGH ALTITUDES UNTIL YOU ARE TOLD THE GAS BUBBLE IS GONE. A rapid increase in altitude can cause a dangerous rise in eye pressure.
What are the risks of surgery?Any surgery has risks; however, an untreated retinal detachment usually results in permanent severe vision loss or blindness.
Some of the surgical risks include:
- Infection
- Bleeding
- High pressure in the eye
- Cataract
Most retinal detachment surgery is successful, although a second operation is sometimes needed.
If the retinal cannot be reattached, then the eye will continue to lose sight and ultimately become blind.
Will your vision improve?Vision may take many months to improve and in some cases may never return fully. Unfortunately, some patients do not recover any vision.
The more severe the detachment, the less vision may return. For this reason, it is very important to see your eye care provider at the first sign of any trouble.
Diabetic Retinopathy
If you have diabetes mellitus, your body does not use and store sugar properly. High blood-sugar (glucose) levels can damage blood vessels in the retina, the nerve layer at the back of the eye that senses light and helps to send images to the brain. The damage to retinal vessels is referred to as diabetic retinopathy.
Types of diabetic retinopathyThere are two types of diabetic retinopathy: nonproliferative diabetic retinopathy (NPDR) and proliferative diabetic retinopathy (PDR).
NPDR, commonly known as background retinopathy, is an early stage of diabetic
retinopathy. In this stage, tiny blood vessels within the retina leak blood or fluid. The leaking fluid causes the retina to swell or to form deposits called exudates.Many people with diabetes have mild NPDR, which usually does not affect their vision. When vision is affected it is the result of macular edema and/or macular ischemia.
Macular edema is swelling, or thickening, of the macula, a small area in the center of the retina that allows us to see fine details clearly. The swelling is caused by fluid leaking from retinal blood vessels. It is the most common cause of visual loss in diabetes. Vision loss may be mild to severe, but even in the worst cases, peripheral vision continues to function.
Macular ischemia occurs when small blood vessels (capillaries) close. Vision blurs because the macula no longer receives sufficient blood supply to work properly.
PDR is present when abnormal new vessels (neovascularization) begin growing on the surface of the retina or optic nerve. The main cause of PDR is widespread closure of retinal blood vessels, preventing adequate blood flow. The retina responds by growing new blood vessels in an attempt to supply blood to the area where the original vessels closed.
Unfortunately, the new, abnormal blood vessels do not resupply the retina with normal blood flow. The new vessels are often accompanied by scar tissue that may cause wrinkling or detachment of the retina.
PDR may cause more severe vision loss than NPDR because it can affect both central and peripheral vision. Proliferative diabetic retinopathy causes visual loss in the following ways:
Vitreous hemorrhage: The fragile new vessels may bleed into the vitreous, a clear, jelly-like substance that fills the center of the eye. If the vitreous hemorrhage is small, a person might see only a few new dark floaters. A very large hemorrhage might block out all vision.
It may take days, months or even years to resorb the blood, depending on the amount of blood present. If the eye does not clear the vitreous blood adequately within a reasonable time, vitrectomy surgery may be recommended. Vitreous hemorrhage alone does not cause permanent vision loss. When the blood clears, visual acuity may return to its former level unless the macula is damaged.
Traction retinal detachment: when PDR is present, scar tissue associated with neovascularization can shrink, wrinkling and pulling the retina from its normal position. Macular wrinkling can cause visual distortion. More severe vision loss can offer if the macula or large areas of the retina are detached.
Neovascular glaucoma: Occasionally, extensive retinal vessel closure will cause new, abnormal blood vessels to grow on the iris (colored part of the eye) and block the normal flow of fluid out of the eye. Pressure in the eye builds up, resulting in neovascular glaucoma, a severe eye disease that causes damage to the optic nerve.
How is diabetic retinopathy diagnosed?A medical eye examination is the only way to find changes inside your eye. An eye care provider can often diagnose and treat serious retinopathy before you are aware of any vision problems. The eye care provider dilates your pupil and looks inside of the eye with a binocular indirect ophthalmoscope.
If your eye care provider finds diabetic retinopathy, he or she may order color photographs of the retina, retinal laser scans using the new OCT3 technology or a special test called fluorescein angiography to find out if you need treatment.
How is diabetic retinopathy treated?The best treatment is to prevent the development retinopathy as much as possible. Strict control of your blood sugar will significantly reduce the long-term risk of vision loss from diabetic retinopathy. If high blood pressure and kidney problems are present, they need to be treated.
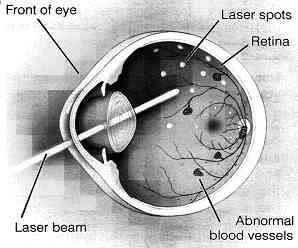
Laser surgery: Laser surgery is often recommended for people with macular edema, PDR and neovascular glaucoma. For macular edema, the laser is focused on the damaged retina near the macula to decrease the fluid leakage. The main goal of treatment is to prevent further loss of vision. It is uncommon for people who have blurred vision from macular edema to recover normal vision, although some may experience partial improvement. A few people may see the laser spots near the center of their vision following treatment. The spots usually fade with time, but may not disappear.
For PDR, the laser is focused on all parts of the retina except the macula. This panretinal photocoagulation treatment causes abnormal new vessels to shrink and often prevents them from growing in the future. It also decreases the chance that vitreous bleeding or retinal distortion will occur. Multiple laser treatments over time are sometimes necessary. Laser surgery does not cure diabetic retinopathy and does not always prevent further loss of vision.
Vitrectomy: In advanced PDR, a diabetic retinal specialist may recommend a vitrectomy. During this microsurgical procedure, which is performed in the operating room, the blood-filled vitreous is removed and replaced with a clear solution. A diabetic retinal specialist may wait for several months or up to a year to see if the blood clears on its own before performing a vitrectomy. Vitrectomy often prevents further bleeding by removing the abnormal vessels that caused the bleeding. If the retina is detached, it can be repaired during the vitrectomy surgery. Surgery should usually be done early because macular distortion or traction retinal detachment will cause permanent visual loss. The longer the macula is distorted or out of place, the more serious the vision loss will be.
Vision loss is largely preventableIf you have diabetes, it is important to know that today, with improved methods of diagnosis and treatment, only a small percentage of people who develop retinopathy have serious vision problems. Early detection of diabetic retinopathy is the best protection against loss of vision.
You can significantly lower your risk of vision loss by maintaining strict control of your blood sugar and visiting your eye care provider regularly.
When to schedule and examinationPeople with diabetes should schedule examinations at lease once a year. More frequent medical eye examinations may be necessary after the diagnosis of diabetic retinopathy.
Pregnant women with diabetes should schedule an appointment in the first trimester because retinopathy can progress quickly during pregnancy.
If you need to be examined for glasses, it is important that your blood sugar be in consistent control for several days when you see your eye care provider. Glasses that work well when the blood sugar is stable may not work well when sugar is out of control.
Rapid changes in blood sugar can cause fluctuating vision in both eyes even if retinopathy is not present.
You should have your eyes checked promptly if you have visual changes that:
- Affect only one eye
- Last more than a few days
- Are not associated with a change in blood sugar
When you are first diagnosed with diabetes, you should have your eyes checked soon to establish a baseline and then yearly.
Floaters & Flashes
You may sometimes see small specks or clouds moving in your field of vision. They are called floaters. You can often see them when looking at a plain background, like a blank wall or a blue sky.
Floaters are actually tiny clumps of gel or cells inside the vitreous, the clear jelly-like fluid that fills the inside of your eye.
While these objects look like they are in front of your eye, they are actually floating inside. What you see are the shadows they cast on the retina, the nerve layer at the back of the eye that senses light and allows you to see. Floaters can have different shapes; little dots, circles, lines, clouds, or cobwebs.
When people reach middle age, the vitreous gel may start to thicken or shrink, forming clumps or strands inside the eye. The vitreous gel pulls away from the back wall of the eye, causing a posterior vitreous detachment. It is a common cause of floaters.
Posterior vitreous detachmentis more common for people who:
- Are nearsighted
- Have undergone cataract operations
- Have had YAG laser surgery of the eye
- Have had inflammation inside the eye
The appearance of floaters may be alarming, especially if they develop suddenly. You should see an eye care professional right away if you suddenly develop new floaters, especially if you are over 45 years of age.
Are floaters ever serious?The retina can tear if the shrinking vitreous gel pulls away from the wall of the eye. This sometimes causes a small amount of bleeding in the eye that may appear as new floaters.
A torn retina is always a serious problem, since it can lead to a retinal detachment. You should see your eye care professional as soon as possible if:
- New floaters appears suddenly
- You see sudden flashes of light
- You notice other symptoms like the loss of side vision
Because you need to know if your retina is torn, call your eye care professional if a new floater appears suddenly.
Floaters can get in the way of clear vision, which may be quite annoying, especially if you are trying to read. You can try moving your eyes, looking up and then down to move the floaters out of the way.
While some floaters may remain in your vision, many of them will fade over time and become less bothersome. Even if you have had some floaters for years, you should have an eye examination immediately if you notice new ones.
What causes flashing lights?When the vitreous gel rubs or pulls on the retina, you may see what look like flashing lights or lightning streaks. You may have experienced this same sensation if you have ever been hit in the eye and seen "stars."
The flashes of light can appear off and on for several weeks or months. As we grow older, it is more common to experience flashes. If you notice the sudden appearance of light flashes, you should visit your eye care professional immediately to see if the retina has been torn.
MigraineSome people experience flashes of light that appear as jagged lines or “heat waves” in both eyes, often lasting 10-20 minutes. These types of flashes are usually caused by a spasm of blood vessels in the brain, which is called migraine.
If a headache follows the flashes, it is called a migraine headache. However, jagged lines or "heat waves" can occur without a headache. In this case, the light flashes are called ophthalmic migraine, or migraine without headache.
How are your eyes examined?When an eye care professional examines your eyes, your pupils may be dilated with eye drops. During this painless examination, your eye care professional will carefully observe your retina and vitreous. If your eyes have been dilated, you may need to make arrangements for someone to drive you home afterwards.
Floaters and flashes of light become more common as we grow older. While not all floaters and flashes are serious, you should always have a medical eye examination by an eye care professional to make sure there has been no damage to your retina.